June 2021
What Are the Different Types of Orthotics?
 Orthotics are devices used on the outside of your body to correct biomechanical problems. Most people are familiar with orthotic insoles, which are over-the-counter or custom-made devices that are placed directly into your shoes. These are often used to treat foot problems such as flat feet and plantar fasciitis. Other types of orthotics include ankle-foot orthoses (AFOs), which are used to hold the foot and ankle in the correct positions and support the ankle, and prescription footwear, which are specially designed shoes used to correct various foot problems. To learn more about orthotics, and to see if they may be right for you, please consult with a podiatrist.
Orthotics are devices used on the outside of your body to correct biomechanical problems. Most people are familiar with orthotic insoles, which are over-the-counter or custom-made devices that are placed directly into your shoes. These are often used to treat foot problems such as flat feet and plantar fasciitis. Other types of orthotics include ankle-foot orthoses (AFOs), which are used to hold the foot and ankle in the correct positions and support the ankle, and prescription footwear, which are specially designed shoes used to correct various foot problems. To learn more about orthotics, and to see if they may be right for you, please consult with a podiatrist.
If you are having discomfort in your feet and would like to try orthotics, contact Dr. Lee R. Stein from Lake Shore Foot & Ankle, PC. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Are Orthotics?
Orthotics are inserts you can place into your shoes to help with a variety of foot problems such as flat feet or foot pain. Orthotics provide relief and comfort for minor foot and heel pain but can’t correct serious biomechanical problems in your feet.
Over-the-Counter Inserts
Orthotics come in a wide variety of over-the-counter inserts that are used to treat foot pain, heel pain, and minor problems. For example, arch supports can be inserted into your shoes to help correct overarched or flat feet, while gel insoles are often used because they provide comfort and relief from foot and heel pain by alleviating pressure.
Prescription Orthotics
If over-the-counter inserts don’t work for you or if you have a more severe foot concern, it is possible to have your podiatrist prescribe custom orthotics. These high-quality inserts are designed to treat problems such as abnormal motion, plantar fasciitis, and severe forms of heel pain. They can even be used to help patients suffering from diabetes by treating foot ulcers and painful calluses and are usually molded to your feet individually, which allows them to provide full support and comfort.
If you are experiencing minor to severe foot or heel pain, it’s recommended to speak with your podiatrist about the possibilities of using orthotics. A podiatrist can determine which type of orthotic is right for you and allow you to take the first steps towards being pain-free.
If you have any questions please contact one of our offices located in Chicago, Highland Park, and Uptown, IL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Seeing a Podiatrist for Plantar Fasciitis
Plantar fasci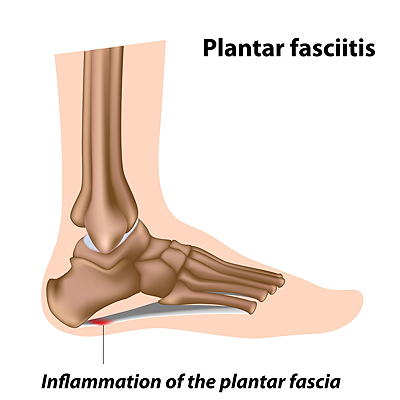 itis is the inflammation of the plantar fascia, which is the band of tissue that runs along the bottom of the foot from the heel to the toes. A common sign of plantar fasciitis is pain in the heel as well as the arch of the foot. The pain is usually worse when taking your first few steps right after sleeping or resting, and it may ease during exercise and worsen afterwards. Common risk factors for plantar fasciitis include exercising with a tight calf, recently starting to exercise on hard surfaces, wearing shoes with poor support, and being overweight. Patients who have heel pain that is stopping them from doing daily activities, that keeps getting worse, has not improved, or who also have diabetes should consult with a podiatrist for a proper diagnosis and treatment for the pain.
itis is the inflammation of the plantar fascia, which is the band of tissue that runs along the bottom of the foot from the heel to the toes. A common sign of plantar fasciitis is pain in the heel as well as the arch of the foot. The pain is usually worse when taking your first few steps right after sleeping or resting, and it may ease during exercise and worsen afterwards. Common risk factors for plantar fasciitis include exercising with a tight calf, recently starting to exercise on hard surfaces, wearing shoes with poor support, and being overweight. Patients who have heel pain that is stopping them from doing daily activities, that keeps getting worse, has not improved, or who also have diabetes should consult with a podiatrist for a proper diagnosis and treatment for the pain.
Plantar fasciitis is a common foot condition that is often caused by a strain injury. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Dr. Lee R. Stein from Lake Shore Foot & Ankle, PC. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is a ligament that connects your heel to the front of your foot. When this ligament becomes inflamed, plantar fasciitis is the result. If you have plantar fasciitis you will have a stabbing pain that usually occurs with your first steps in the morning. As the day progresses and you walk around more, this pain will start to disappear, but it will return after long periods of standing or sitting.
What Causes Plantar Fasciitis?
- Excessive running
- Having high arches in your feet
- Other foot issues such as flat feet
- Pregnancy (due to the sudden weight gain)
- Being on your feet very often
There are some risk factors that may make you more likely to develop plantar fasciitis compared to others. The condition most commonly affects adults between the ages of 40 and 60. It also tends to affect people who are obese because the extra pounds result in extra stress being placed on the plantar fascia.
Prevention
- Take good care of your feet – Wear shoes that have good arch support and heel cushioning.
- Maintain a healthy weight
- If you are a runner, alternate running with other sports that won’t cause heel pain
There are a variety of treatment options available for plantar fasciitis along with the pain that accompanies it. Additionally, physical therapy is a very important component in the treatment process. It is important that you meet with your podiatrist to determine which treatment option is best for you.
If you have any questions, please feel free to contact one of our offices located in Chicago, Highland Park, and Uptown, IL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
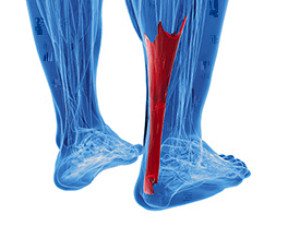
What an Achilles Tendon Injury May Feel Like
At the lower end of the calf, the two calf muscles (gastrocnemius and soleus) join and become one long band of fibrous tissue known as the Achilles tendon. The Achilles tendon connects the calf with the heel and helps the foot bend. The Achilles tendon may become injured, torn, or ruptured during physical activities that involve sudden starts and stops, jumping or running. It can also occur during regular activities in people aged 40-64 who have diabetes, high cholesterol, or a problem with weight. A snapping, cracking, or popping sound may occur at the moment of injury or when pressure is applied to the damaged tendon. Other symptoms may include: pain, swelling, bruising, or stiffness in the back of the foot and tendon area—which can be worse upon waking or after exercise—a weakened leg, reduced mobility, or sensitivity to touch. If you suspect you may have injured your Achilles tendon, seek the care of a podiatrist to receive an accurate diagnosis and treatment.
Achilles tendon injuries need immediate attention to avoid future complications. If you have any concerns, contact Dr. Lee R. Stein of Lake Shore Foot & Ankle, PC. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is the Achilles Tendon?
The Achilles tendon is a tendon that connects the lower leg muscles and calf to the heel of the foot. It is the strongest tendon in the human body and is essential for making movement possible. Because this tendon is such an integral part of the body, any injuries to it can create immense difficulties and should immediately be presented to a doctor.
What Are the Symptoms of an Achilles Tendon Injury?
There are various types of injuries that can affect the Achilles tendon. The two most common injuries are Achilles tendinitis and ruptures of the tendon.
Achilles Tendinitis Symptoms
- Inflammation
- Dull to severe pain
- Increased blood flow to the tendon
- Thickening of the tendon
Rupture Symptoms
- Extreme pain and swelling in the foot
- Total immobility
Treatment and Prevention
Achilles tendon injuries are diagnosed by a thorough physical evaluation, which can include an MRI. Treatment involves rest, physical therapy, and in some cases, surgery. However, various preventative measures can be taken to avoid these injuries, such as:
- Thorough stretching of the tendon before and after exercise
- Strengthening exercises like calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses
If you have any questions please feel free to contact one of our offices located in Chicago, Highland Park, and Uptown, IL . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Arthritis Can Cause Pain in the Feet and Ankles
Tips to Prevent Running Injuries
If you are a runner, then you are likely no stranger to foot and ankle injuries. Running can put immense strain on the lower limbs, leading to conditions such as plantar fasciitis, Achilles tendinitis, ankle strains and sprains, and stress fractures. Fortunately, there are steps that you can take to avoid foot and ankle injuries while running. The most important thing you can do to prevent injuries is train slowly. Increase the mileage, duration, or intensity of your runs separately and gradually over time, and give yourself plenty of time to rest following a run. It is also important that you wear properly fitted shoes that support and protect your feet. For more information about preventing running injuries, please speak with a podiatrist.
Exercising your feet regularly with the proper foot wear is a great way to prevent injuries. If you have any concerns about your feet, contact Dr. Lee R. Stein of Lake Shore Foot & Ankle, PC. Our doctor will treat your foot and ankle needs.
How to Prevent Running Injuries
Many common running injuries are caused by overuse and overtraining. When the back of the kneecap starts wearing out and starts causing pain in your knee, this is commonly referred to as runner’s knee. Runner’s knee is a decrease in strength in your quadriceps and can occur if you’re not wearing properly fitted or supporting shoes. To prevent runner’s knee, focusing on hip strengthening is a good idea, as well as strengthening your quads to keep the kneecaps aligned.
What Are Some Causes of Running Injuries?
- One cause of a common running injury is called iliotibial band syndrome.
- Plantar fasciitis is also another common injury.
- Stress fractures can occur from overtraining, lack of calcium, or even your running style.
Best Ways to Prevent Running Injuries
- Wear footwear that fits properly and suits your running needs.
- Running shoes are the only protective gear that runners have to safeguard them from injury.
- Make a training schedule. Adding strengthening exercises as well as regular stretching can help keep you strong and limber and can lessen the possibility of injuries.
- Stretching keeps muscles limber; this will help you gain better flexibility.
If you have any questions please feel free to contact one of our offices located in Chicago, Highland Park, and Uptown, IL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Plantar Warts: Common, Contagious, and Communal
When the common human papillomavirus (HPV) enters the skin of the foot through a small cut or compromised area and causes keratin to develop, plantar warts occur. These are rough, white, or skin-colored warts that present on the heel, toes, or other weight-bearing points on the sole of the foot. Plantar warts, also known as verrucas, will sometimes have black dots at their core, which are actually clotted blood vessels. Because HPV is contagious, plantar warts can be passed from the skin of one person to another through direct contact, or by indirect exposure to an infected person’s socks, shoes, towels, or surfaces such as public swimming pools or communal changing rooms where the virus may be living. The virus can spread to hands and fingers, but the warts that develop on these parts of the body are known as palmar warts. People with a weakened immune system, diabetes, HIV/AIDS, or those who have warts that bleed, change color, cause a loss of sensation in the foot, or are very painful, should seek professional help. A podiatrist has a variety of remedies and procedures that can treat or even remove plantar warts.
Plantar warts can be very uncomfortable. If you need your feet checked, contact Dr. Lee R. Stein from Lake Shore Foot & Ankle, PC. Our doctor will assist you with all of your foot and ankle needs.
About Plantar Warts
Plantar warts are the result of HPV, or human papillomavirus, getting into open wounds on the feet. They are mostly found on the heels or balls of the feet.
While plantar warts are generally harmless, those experiencing excessive pain or those suffering from diabetes or a compromised immune system require immediate medical care. Plantar warts are easily diagnosed, usually through scraping off a bit of rough skin or by getting a biopsy.
Symptoms
- Lesions on the bottom of your feet, usually rough and grainy
- Hard or thick callused spots
- Wart seeds, which are small clotted blood vessels that look like little black spots
- Pain, discomfort, or tenderness of your feet when walking or standing
Treatment
- Freezing
- Electric tool removal
- Laser Treatment
- Topical Creams (prescription only)
- Over-the-counter medications
To help prevent developing plantar warts, avoid walking barefoot over abrasive surfaces that can cause cuts or wounds for HPV to get into. Avoiding direct contact with other warts, as well as not picking or rubbing existing warts, can help prevent the further spread of plantar warts. However, if you think you have developed plantar warts, speak to your podiatrist. He or she can diagnose the warts on your feet and recommend the appropriate treatment options.
If you have any questions please feel free to contact one of our offices located in Chicago, Highland Park, and Uptown, IL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Blog Archives
- April 2025
- March 2025
- February 2025
- January 2025
- December 2024
- November 2024
- October 2024
- September 2024
- August 2024
- July 2024
- June 2024
- May 2024
- April 2024
- March 2024
- February 2024
- January 2024
- December 2023
- November 2023
- October 2023
- September 2023
- August 2023
- July 2023
- June 2023
- May 2023
- April 2023
- March 2023
- February 2023
- January 2023
- December 2022
- November 2022
- October 2022
- September 2022
- August 2022
- July 2022
- June 2022
- May 2022
- April 2022
- March 2022
- February 2022
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018