Recovering From Tenosynovitis
Tenosynovitis is an inflammation of a tendon and its synovium, or lining. This condition can affect the feet or ankles and occur due to injury, repetitive overuse, excessive pressure on the tendon, or an infection. Tenosynovitis usually affects athletes, ballet dancers, and older adults. While recovering from this condition, it is suggested that you limit your leg and foot movement to decrease stress on the tendon and prevent further damage. Applying ice or heat to the area can help reduce swelling and pain. At home, you may need to wear a splint, brace, or walking boot, and may need crutches to get around. It is important to follow your doctor’s instructions so that you can recover fully and return to your usual activities as soon as possible. If you are experiencing ankle pain, please consult with a podiatrist.
Ankle pain can have many different causes and the pain may potentially be serious. If you have ankle pain, consult with Dr. Lee R. Stein from Lake Shore Foot & Ankle, PC. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Ankle pain is any condition that causes pain in the ankle. Due to the fact that the ankle consists of tendons, muscles, bones, and ligaments, ankle pain can come from a number of different conditions.
Causes
The most common causes of ankle pain include:
- Types of arthritis (rheumatoid, osteoarthritis, and gout)
- Ankle sprains
- Broken ankles
- Achilles tendinitis
- Achilles tendon rupture
- Stress fractures
- Tarsal tunnel syndrome
- Plantar fasciitis
Symptoms
Symptoms of ankle injury vary based upon the condition. Pain may include general pain and discomfort, swelling, aching, redness, bruising, burning or stabbing sensations, and/or loss of sensation.
Diagnosis
Due to the wide variety of potential causes of ankle pain, podiatrists will utilize a number of different methods to properly diagnose ankle pain. This can include asking for personal and family medical histories and of any recent injuries. Further diagnosis may include sensation tests, a physical examination, and potentially x-rays or other imaging tests.
Treatment
Just as the range of causes varies widely, so do treatments. Some more common treatments are rest, ice packs, keeping pressure off the foot, orthotics and braces, medication for inflammation and pain, and surgery.
If you have any questions, please feel free to contact one of our offices located in Chicago, Highland Park, and Uptown, IL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Ankle Pain
The ankle joint is the point at which the bones of the leg and foot join. This joint is crucial because it is responsible for the foot’s mobility. Ankle pain is typically the result of inflammation from an injury to bones, joint space, cartilage, ligaments, tendons, or muscles in the area. Commonly associated symptoms with ankle pain are bruising, redness, numbness, stiffness, weakness, and tingling.
The most common causes of ankle pain are sprains and injuries. Ankle sprains are one of the most common musculoskeletal injuries. Sprains occur when the ligaments of the ankle become partially or completely torn due to sudden stretching. Sprains can occur on either the inner or outer sides of the ankle joint. Usually, these injuries occur when the ankle is twisted in an activity by stepping off an uneven surface. More specific causes include rheumatoid arthritis, gout, osteoarthritis, and Achilles tendonitis.
If you are experiencing ankle pain, you should consult with your podiatrist to choose the best method of care. Your doctor will conduct an examination of your ankle to determine the underlying cause of the pain.
The Wagner Diabetic Foot Ulcer Classification System
If you suffer from diabetes, you may be familiar with the increased risk of developing poorly healing wounds on your feet. Small cuts, sores, or scrapes can go unnoticed due to neuropathy or nerve damage, and heal slowly because of poor circulation. These issues can make wounds grow larger and become infected, turning into diabetic foot ulcers (DFUs). There are various classification systems for describing the general characteristics of these wounds. Doctors who use the Wagner system classify DFUs by their severity, in a graded system ranging from 0 to 5. A Grade 0 ulcer means that the skin is intact. Grade 1 signifies a superficial ulcer on the outer layers of skin. Grade 2 is a deep ulcer. Grade 3 is an ulcer with bone involvement. Grade 4 means that there is gangrene or dead tissue in the front of the foot, while Grade 5 means that the gangrene has spread to the entire foot. If you notice any wounds on your feet, please schedule an appointment with a podiatrist who can treat wounds and help you manage your condition.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with Dr. Lee R. Stein from Lake Shore Foot & Ankle, PC. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact one of our offices located in Chicago, Highland Park, and Uptown, IL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Wound Care
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a doctor—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.
Sesamoid Bones and Injuries
The sesamoids are two small, pea-shaped bones found just under the base of the big toe. The sesamoids are embedded in a tendon, allowing you to move the big toes and acting as shock absorbers in the foot while you walk and run. Though these bones are quite small, they can be easily injured. The area around the sesamoid bones may become inflamed due to injury or overuse, leading to sesamoiditis. Over time, these bones may become unable to bear the load placed on them and could even develop tiny stress fractures. A sudden injury to the bones can cause them to fully fracture. If you have pain, swelling, or bruising in the ball of your foot, schedule an appointment with a podiatrist who can diagnose and treat various sesamoid injuries.
Sesamoiditis is an unpleasant foot condition characterized by pain in the balls of the feet. If you think you’re struggling with sesamoiditis, contact Dr. Lee R. Stein of Lake Shore Foot & Ankle, PC. Our doctor will treat your condition thoroughly and effectively.
Sesamoiditis
Sesamoiditis is a condition of the foot that affects the ball of the foot. It is more common in younger people than it is in older people. It can also occur with people who have begun a new exercise program, since their bodies are adjusting to the new physical regimen. Pain may also be caused by the inflammation of tendons surrounding the bones. It is important to seek treatment in its early stages because if you ignore the pain, this condition can lead to more serious problems such as severe irritation and bone fractures.
Causes of Sesamoiditis
- Sudden increase in activity
- Increase in physically strenuous movement without a proper warm up or build up
- Foot structure: those who have smaller, bonier feet or those with a high arch may be more susceptible
Treatment for sesamoiditis is non-invasive and simple. Doctors may recommend a strict rest period where the patient forgoes most physical activity. This will help give the patient time to heal their feet through limited activity. For serious cases, it is best to speak with your doctor to determine a treatment option that will help your specific needs.
If you have any questions please feel free to contact one of our offices located in Chicago, Highland Park, and Uptown, IL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Sesamoiditis
Sesamoiditis is a condition in which the sesamoid bones in the forefoot become inflamed from physical activity. Sesamoid bones are bones that are not connected to other bones but are located in tendons or muscle. Two of these sesamoid bones are very small and located on the underside of the foot near the big toe. Athletes such as runners, baseball and football players, and dancers are likely to experience sesamoiditis. Those with high arched feet, flat feet, or runners who run on the ball of their foot are also prone to suffer from sesamoiditis.
Symptoms include pain or throbbing on the ball of the foot near the big toe. The pain generally starts with a mild throbbing but gradually builds up to shooting pain. Bruising, swelling, and redness are possible, but in most cases, these symptoms are not present. However, moving the big toe can result in pain and difficulty.
To conduct a diagnosis, the podiatrist will examine the ball of the foot and big toe. They will look for any outliers and check the movement of the toe. X-rays will be taken to rule out any other conditions and ensure that it is sesamoiditis.
Treatment for sesamoiditis is generally mild and includes rest, anti-inflammatory and pain medication, and ice treatments to deal with the swelling and pain. Orthotics may be needed with people who have flat or high arched feet to relieve pressure off the bones. In some cases the toe will be taped and immobilized to allow healing. The podiatrist may also decide to use a steroid injection to help with swelling as well. If you have sesamoiditis, you shouldn’t engage in any intensive activity, as it may inflame the area and worsen your pain. If the sesamoid bone has fractured, surgery may be required to remove the sesamoid bone.
If you are suffering from sesamoiditis or are experiencing symptoms similar to sesamoiditis, you should stop all physical activity that puts strain on the area. Furthermore you should see a podiatrist for a diagnosis to see if you have sesamoiditis.
What Are the Different Types of Orthotics?
 Orthotics are devices used on the outside of your body to correct biomechanical problems. Most people are familiar with orthotic insoles, which are over-the-counter or custom-made devices that are placed directly into your shoes. These are often used to treat foot problems such as flat feet and plantar fasciitis. Other types of orthotics include ankle-foot orthoses (AFOs), which are used to hold the foot and ankle in the correct positions and support the ankle, and prescription footwear, which are specially designed shoes used to correct various foot problems. To learn more about orthotics, and to see if they may be right for you, please consult with a podiatrist.
Orthotics are devices used on the outside of your body to correct biomechanical problems. Most people are familiar with orthotic insoles, which are over-the-counter or custom-made devices that are placed directly into your shoes. These are often used to treat foot problems such as flat feet and plantar fasciitis. Other types of orthotics include ankle-foot orthoses (AFOs), which are used to hold the foot and ankle in the correct positions and support the ankle, and prescription footwear, which are specially designed shoes used to correct various foot problems. To learn more about orthotics, and to see if they may be right for you, please consult with a podiatrist.
If you are having discomfort in your feet and would like to try orthotics, contact Dr. Lee R. Stein from Lake Shore Foot & Ankle, PC. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Are Orthotics?
Orthotics are inserts you can place into your shoes to help with a variety of foot problems such as flat feet or foot pain. Orthotics provide relief and comfort for minor foot and heel pain but can’t correct serious biomechanical problems in your feet.
Over-the-Counter Inserts
Orthotics come in a wide variety of over-the-counter inserts that are used to treat foot pain, heel pain, and minor problems. For example, arch supports can be inserted into your shoes to help correct overarched or flat feet, while gel insoles are often used because they provide comfort and relief from foot and heel pain by alleviating pressure.
Prescription Orthotics
If over-the-counter inserts don’t work for you or if you have a more severe foot concern, it is possible to have your podiatrist prescribe custom orthotics. These high-quality inserts are designed to treat problems such as abnormal motion, plantar fasciitis, and severe forms of heel pain. They can even be used to help patients suffering from diabetes by treating foot ulcers and painful calluses and are usually molded to your feet individually, which allows them to provide full support and comfort.
If you are experiencing minor to severe foot or heel pain, it’s recommended to speak with your podiatrist about the possibilities of using orthotics. A podiatrist can determine which type of orthotic is right for you and allow you to take the first steps towards being pain-free.
If you have any questions please contact one of our offices located in Chicago, Highland Park, and Uptown, IL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Foot Orthotics
Orthotics are shoe inserts that are meant to correct an irregular walking gait or provide cushioning to the feet. Orthotics come in a variety of different models and sizes, including over-the-counter and customizable variants. Customizable orthotics can be shaped and contoured to fit inside a specific shoe and are typically prescribed through a podiatrist who specializes in customized footwear and orthotics design and management.
Orthotics are beneficial because they can help prevent injuries from occurring and provide cushioning to keep pain levels down to a minimum. They also allow for the correct positioning of the feet. Orthotics can act as shock absorbers to help remove pressure from the foot and ankle. Therefore, orthotics can make bodily movements, such as walking and running, become more comfortable as well as help prevent the development of certain foot conditions.
Orthotics alleviate pain and make the foot more comfortable by slightly altering the angle at which the foot strikes the ground surface, therefore controlling the movement of the foot and ankle. Orthotics come in different variants and can be made of various materials. To determine what type of orthotic is most suited to your feet and your needs, it is best to consult your podiatrist. He or she will be able to recommend a type of orthotic that can help improve your foot function or prescribe a custom orthotic to best fit your feet.
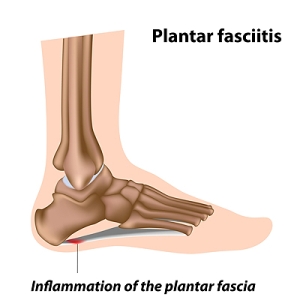
Seeing a Podiatrist for Plantar Fasciitis
Plantar fasci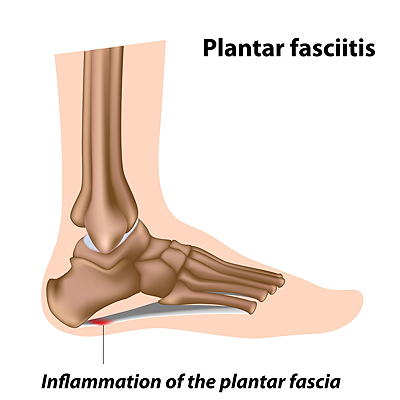 itis is the inflammation of the plantar fascia, which is the band of tissue that runs along the bottom of the foot from the heel to the toes. A common sign of plantar fasciitis is pain in the heel as well as the arch of the foot. The pain is usually worse when taking your first few steps right after sleeping or resting, and it may ease during exercise and worsen afterwards. Common risk factors for plantar fasciitis include exercising with a tight calf, recently starting to exercise on hard surfaces, wearing shoes with poor support, and being overweight. Patients who have heel pain that is stopping them from doing daily activities, that keeps getting worse, has not improved, or who also have diabetes should consult with a podiatrist for a proper diagnosis and treatment for the pain.
itis is the inflammation of the plantar fascia, which is the band of tissue that runs along the bottom of the foot from the heel to the toes. A common sign of plantar fasciitis is pain in the heel as well as the arch of the foot. The pain is usually worse when taking your first few steps right after sleeping or resting, and it may ease during exercise and worsen afterwards. Common risk factors for plantar fasciitis include exercising with a tight calf, recently starting to exercise on hard surfaces, wearing shoes with poor support, and being overweight. Patients who have heel pain that is stopping them from doing daily activities, that keeps getting worse, has not improved, or who also have diabetes should consult with a podiatrist for a proper diagnosis and treatment for the pain.
Plantar fasciitis is a common foot condition that is often caused by a strain injury. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Dr. Lee R. Stein from Lake Shore Foot & Ankle, PC. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is a ligament that connects your heel to the front of your foot. When this ligament becomes inflamed, plantar fasciitis is the result. If you have plantar fasciitis you will have a stabbing pain that usually occurs with your first steps in the morning. As the day progresses and you walk around more, this pain will start to disappear, but it will return after long periods of standing or sitting.
What Causes Plantar Fasciitis?
- Excessive running
- Having high arches in your feet
- Other foot issues such as flat feet
- Pregnancy (due to the sudden weight gain)
- Being on your feet very often
There are some risk factors that may make you more likely to develop plantar fasciitis compared to others. The condition most commonly affects adults between the ages of 40 and 60. It also tends to affect people who are obese because the extra pounds result in extra stress being placed on the plantar fascia.
Prevention
- Take good care of your feet – Wear shoes that have good arch support and heel cushioning.
- Maintain a healthy weight
- If you are a runner, alternate running with other sports that won’t cause heel pain
There are a variety of treatment options available for plantar fasciitis along with the pain that accompanies it. Additionally, physical therapy is a very important component in the treatment process. It is important that you meet with your podiatrist to determine which treatment option is best for you.
If you have any questions, please feel free to contact one of our offices located in Chicago, Highland Park, and Uptown, IL . We offer the newest diagnostic and treatment technologies for all your foot care needs.